Graft vs Host Disease
The transplant was successful. But that’s just the beginning…

It sounds like something out of a horror film. And to be honest, it’s the stuff nightmares are made of. In a transplant, the Graft is the donor’s stem cells which are put into the Host, who is the recipient. The new cells still have part of the donor’s immune system, and they do what healthy cells are supposed to do: attack the foreign invader. Unfortunately, the new cells sometimes recognize the recipient as the foreign invader and begin to attack several of the systems within the body, causing rampant inflammation.
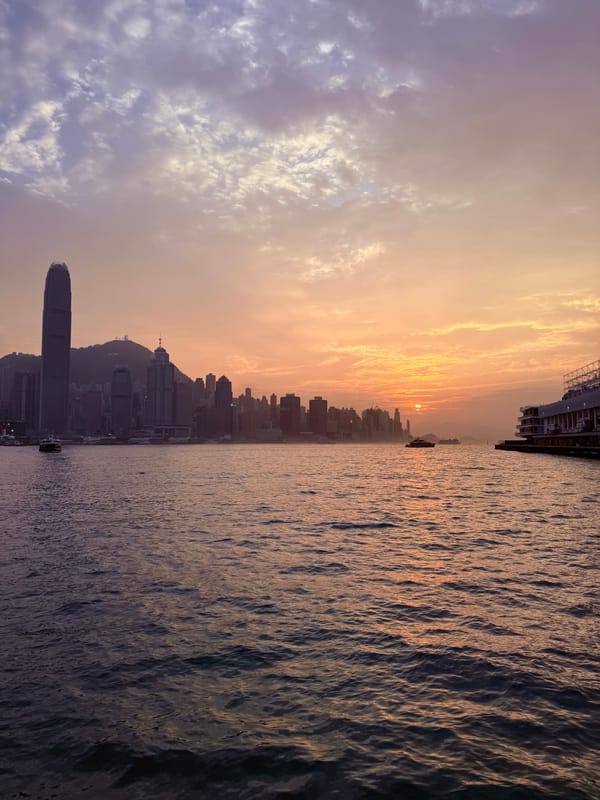
The day Michael and I had the multi-hour informational conference with the transplant team at Queen Mary Hospital, much of the time was spent talking about Graft vs Host Disease (GVHD). There are two types, Acute and Chronic. Much like the types of Leukemia, Acute comes on quick and strong and Chronic develops over time and may stick with you in the long term. Both can cause permanent damage ranging from mild to catastrophic.
For Acute GVHD, the three main systems affected are the skin, the liver, and the gastrointestinal tract. Within days of the transplant, Michael began to have tiny pink dots on the trunk of his body, so faint we questioned whether it was really a rash until the doctor pointed it out as being the first signs of GVHD. They immediately jumped into treatment with immunosuppressant medications.
Next up for Michael were gastrointestinal issues. These range from unpleasant to worrisome, and just the sight of food has become triggering for him. To be absolutely certain it is GVHD and not a viral or bacterial infection of the gut, every possible test has been run. They have also treated him as if the gastro issues are actually an infection, just to rule out any possible bug. But nothing at all has made anything better, so it’s definitely the GVHD.
And then finally liver issues started showing up on his daily blood tests. This is when things move from manageable to serious.
Graft Vs Host Disease is graded from 1 (mild) to 4 (very severe). While the skin alone was Grade 1 and the gut issues on their own were 1 to 2, when you take both of those and throw in liver, it automatically raises the grading to a 3, severe. Again, this is the balancing act part of the transplant process — they want to suppress Michael’s immune system just enough to make it less of a target for attack from the new stem cells, but not so much that the new cells don’t learn to focus on real threats. While they had been treating Michael with immunosuppressive medications and a high dose of steroids, his team of doctors quickly decided it was necessary to jump to a stronger treatment to stop the GVHD progression, which acts like dominos causing issues in other parts of the body.
They recommended a medication called Ruxolitinib, which can help when steroids aren’t working. Most of the time, we aren’t automatically told exactly what they are giving Michael or how much it costs, they just bring in a new IV or hand him a new pill to take. We don’t worry because most of his treatment is covered under the Hong Kong Government subsidy, something we qualify for as Hong Kong residents. But with the Ruxolitinib, they did tell us, because like the TKI inhibitor medication, this drug is not covered by the government subsidy. I had to run down to the hospital pharmacy and pay out of pocket for it. The new drug was a stunning amount of money… four pills were $2,239 HKD, which is about $285 USD.

They planned to start him off with half a pill per day, so four pills would have covered eight days (at $280 HKD/ $35 USD a day). After a week on the new medication without seeing the kind of dramatic changes they’d hoped for, his transplant team decided to up the dose to a full pill per day ($560 HKD / $70 USD a day). Now I buy it in two week increments. We’ve been told he’ll need it for about three months, with the medication being adjusted down as time passes.
Currently, the skin rash part of the GVHD has faded away, leaving what looks like a splotchy dark tan which then begins to peel. This is considered a good sign that it is getting ready to leave. The liver function has stabilized as well, which is a huge relief. The gut issues persist. And they are truly awful! Frustrating, traumatizing, demoralizing, miserable, discouraging… all feelings Michael has experienced sometimes in a single hour!
While this has been a trial for certain, the lead doctor gave us a significant and unexpected favor: instead of keeping to the strict two hour visiting window, he is allowing me to extend my visits as necessary. This has been extraordinarily helpful. As of today Michael has been in isolation for 42 days, and two hours a day just isn’t enough time to get all the things done that he needs help with, let alone time to just sit in each other’s presence.
I wanted to update you earlier, and did indeed start this nearly a week ago, but there’s only so many ways to say this is really difficult and we are all struggling together and individually. Michael’s youngest sister Heidi has once again flown in from America and we are currently working like crazy to prepare our flat for Michael to come home. We have four pages of safety rules and best practice guidelines to cover daily life at home for severely immunocompromised transplant patients, and we’ll need to follow most of them for at least a year, some of them forever. It’s overwhelming, especially considering Michael has an entire team of a dozen people caring for him on a daily basis and at home we have… well, me and our sons and a tiny poodle which will no longer be allowed to sleep in our room or sit on Michael’s lap. Like I said, there’s only so many ways to say this is really difficult.
Thank you for the encouragement and kind words and constant prayer. We are incredibly grateful. More soon!

Like this content and want to support more of it? Consider a one time contribution at Buy Me A Coffee. Thank you and have a Plucky Day!