Michael’s Medical Journal
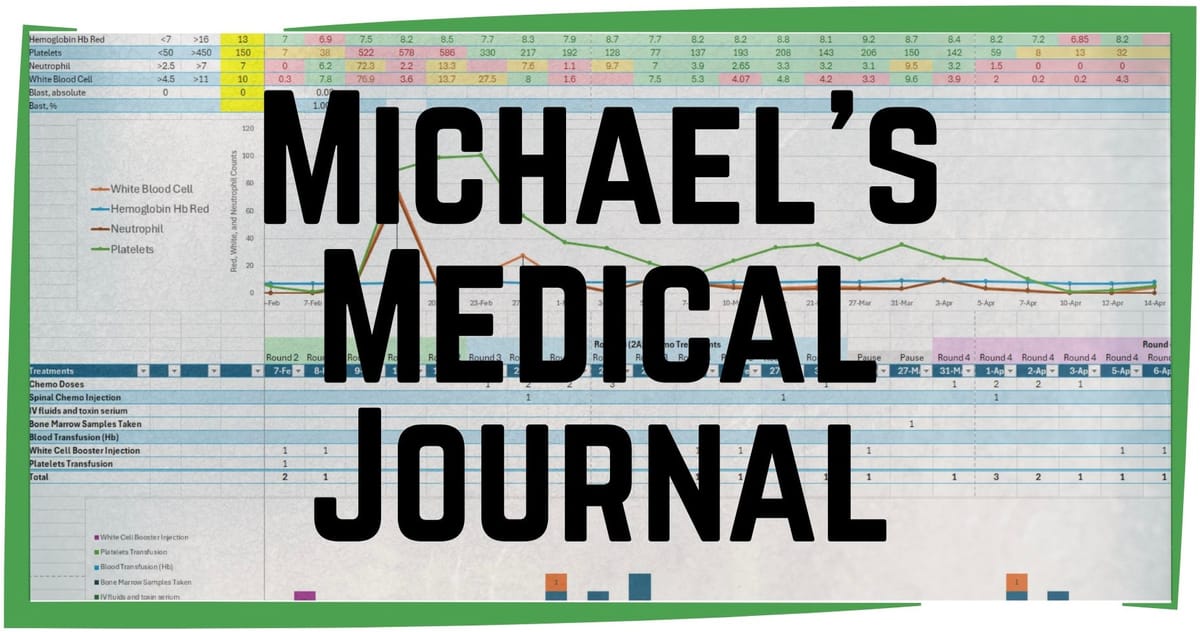
Let’s dive into the details of my cancer treatment. I’m a project manager who deals with data and deadlines. Not much about this has gone according to plan, but I’m recording it all.
I’m just coming to the end of Round Four (of an expected eight rounds) of my chemotherapy treatments. Each round is approximately 24 days long: one to two weeks as an inpatient at Princess Margaret Hospital, followed by two to three weeks at home to recover.
Due to my mixed leukemia type (with both Myeloid and Lymphoblastic origins), each round alternates between two types of chemotherapy treatments, four of each. Let’s call them A and B. Currently, I’m completing a B chemotherapy treatment and getting ready to start another A treatment for Round Five. So it looks like 1A, 2B, 3A, 4B, 5A, 6B, 7A, 8B.
The actual duration of my hospital stays vary depending on how my body reacts to the chemotherapy. For my third round they discharged me after only five days, but on a followup visit I had a fever, so they immediately readmitted me for seven days until the fever was under control. Secondary infections are serious issues and anything can interrupt the plan.
Daily Hospital Schedule
The schedule on the Hematology Ward is predictable and repetitive, and very busy.
6:30 am - lights on, blood pressure and temperature check
7:00 am - morning medication delivered
8:00 am - breakfast tray arrives (porridge or oatmeal)
8:30 am - breakfast tray removed
9:00 am - custodial staff cleans bathroom
10:00 am - morning rounds begins, every patient gets at least a brief visit from the staff doctor
11:00 am - custodial staff cleans room by vigorously wiping down all cabinets, tables, trays, surfaces in each patents bed area prior to visiting hours.
11:30 am - 1:00 pm - morning visiting hours (Heather visit)
11:30 am - midday pills delivered
12:00 pm - lunch tray delivered (removed after 30 minutes)
1:30 pm - cleaning crew again, wipe down everything (after visiting hours)
2:00 pm - blood pressure and temperature check
4:00 pm - cleaning crew again, wipe down everything (in advance of visiting hours)
5:00 pm - 7:30 pm - evening visiting hours (Heather visit)
6:00 pm - evening medication delivered
6:30 pm - dinner tray delivered (removed after 30 minutes)
8:00 pm - post-visiting hours cleaning crew wipes everything down again
9:00 pm - blood pressure and temperature check
11:00 pm - lights out
1:30 am - blood pressure and temperature check
In addition, there are multiple ad hoc visits from nursing staff to collect fluids, administer injections, hook up IV’s, etc.
Round Four Chemotherapy Schedule
A summary of what Round Four looked like:
Thursday March 27 (3 days before chemo starts) — admitted to Hematology Ward at Princess Margaret Hospital as scheduled at 8:30 a.m. No room has an open spot, so I get a bed in the hallway. A blood draw shows all my counts lower than before. I always write down my Hemoglobin (Hb), Platelet, Neutrophil, and White Blood Counts (WBC). A nurse changes the dressing on my PICC line (Peripherally Inserted Central Catheter, a type of IV which goes from my inner arm to the large central veins near my heart), which is done every seven days to prevent infection. A bone marrow sample is taken from the back of my hipbone (a very unpleasant experience) and then I must lay flat for four hours. The first dose of chemo is meant to start today, but due to logistics with the lab and pharmacy, they postpone it until Monday. I am allowed “home leave” over the weekend (not a discharge) and told to return Sunday evening so the first dose of chemo can start early the next morning. We collect three days of medication at the hospital pharmacy and then take a taxi home.
Sunday March 30 (day before chemo starts) — return back to the Hematology Ward at 8:00 pm. Still no room with an open bed, so I’m back in the hallway.
Monday March 31 (Chemo Day 1) — Blood draw shows Hb and Platelets up, Neutrophils and WBC down. Chemo begins at 5:00 am, a single bag on a slow drip that lasts 24 hours. A bed in a room opens up, so I’m moved into a room with two other men. One of them is a previous roommate from back in December. The doctor does rounds and I tell them about back pain and swollen ankles, both side effects of treatment. I’m told to measure all intake and output of fluid for this round of chemotherapy. They start a saline drip to flush some of the chemo, which will be done four times each day they administer chemotherapy.
Tuesday April 1 (Day 2) — My favorite doctor does rounds today (she is kind, soft-spoken, earnest), we discuss back pain and swelling ankles. I’m given a spinal injection (intrathecal chemotherapy) so the cancer-fighting drugs can get into the cerebrospinal fluid which surrounds my brain and spinal cord (an unpleasant experience). Once again, I must lay flat for four hours. I become very dizzy in the afternoon, which resolves around midnight. At 6:30 pm I’m given a steroid treatment then my second bag of chemo begins. Late in the evening I’m given an anti-toxin serum through my PICC line to counteract the negative effects of the chemo. The saline drip continues.
Wednesday April 2 (Day 3)
- Steroid treatment at 7:30 am
- Chemo bag at 8:30 am
- During rounds with the doctor I mention my back pain again, an X-ray is scheduled
- I’m taken to another block for a back X-ray at 2:00 pm
- Steroid treatment at 6:30 pm
- Chemo bag at 7:30 pm
- 500ml saline solution to flush away chemo treatments (4x per day)
- Late evening dose of anti-toxin serum in IV to counteract chemo
Thursday April 3 (Day 4)
- Blood draw 8:00 am (Hb and Platelets down, Neutrophils and WBC up)
- Steroid treatment at 8:30 am
- Chemo bag at 9:30 am (final IV bag for this round)
- Low fever 37.8C (100F)
- Symptoms I’ve experienced overnight and through the morning: acidy hiccups, stuffy nose, throat tight/swollen, watery eyes, swollen face, hands and ankles.
- During rounds with the doctor we discuss that I’ve gained 5kg (11lbs) from fluid retention (I am getting 2 liters of fluids per day in IV). My face, hands and feet have swollen. They will give me something to help flush the fluids out of my system (it will increase urine output, which they are still tracking). Nothing of concern shows on back X-ray.
Friday April 4 (Day 5)
- During rounds with the doctor we discuss my post-chemo symptoms, including a fever, gastrointestinal discomfort, and feeling generally sick. The back pain continues to increase, so I am given Panadol (acetaminophen/paracetamol).
- Concerned with possible infection, they take a urine sample, blood draw, and do a bed-side chest X-ray at 11:00 pm.
Saturday April 5 (Day 6)
- Blood draw 8:00 am (all levels down)
- Rounds today are with the doctor who initially diagnosed my subtype of Leukemia and Ph+ mutation. We discuss my gastro symptoms and fever. She prescribes antibiotics.
- Lab results show low potassium, so they give me two salty potassium supplements to drink.
- WBC is too low, so I’m given a booster injection.
- Still concerned about infection, they take me to another block for chest X-ray.
- No more IV fluids needed.
Sunday April 6 (Day 7)
- WBC injection (boost low white blood cell counts)
- Repeat X-ray again
- Rounds with a new doctor from team, no issues found on X-rays, no mouth sores (something they check for each day as a side effect of chemotherapy), starting to eat better, developed a rash, probably due to steroids.
- Asked for a change of bedding and new PJ’s since I’m not hooked up to an IV anymore.
Monday April 7 (Day 8)
- Blood draw 7:00 am (all levels continue falling)
- Second spinal injection (intrathecal chemotherapy) for this round, always scheduled for Days 2 and 8. I lay flat for four hours and then my head begins to hurt (side effect from puncturing the spinal cord), nausea rises until I begin vomiting through the evening. Low fever in the morning, so they won’t discharge me today.
Tuesday April 8 (Day 9) Discharge!
- During rounds with doctor I learn my body weight is almost back to admission level (fluid retention has subsided). The bone marrow sample results are not back from the lab yet. I have signs of bruising from the low level of platelets. I’m given a cream for the rash, told not to scratch (infection is a risk). No fever in last 24 hours, so they will discharge me today!
- Discharge paperwork, pharmacy prescription and return appointments made for Thursday, Saturday, and Monday.
- Heather arrives and we go home at noon. I sleep in my own bed at night!
Thursday April 10 (Day 11) Day Ward
- I report to the Day Ward at Princess Margaret Hospital where they draw my blood at 9:00 am and then I wait 2-3 hours for the results. All my numbers are low, especially my platelets which are in single digits (normal is between 150-400). My wrist has a bruise from just the pressure of wearing my watch. No fever.
- Due to the dangerously low platelets, I’m given a plasma transfusion and then I can go home.
Saturday April 12 (Day 13) Day Ward
- Back at the Day Ward I have a blood draw at 9:00 am and then wait 2-3 hours for results. The normally busy, packed Day Ward is empty this Saturday, more staff than patients! Platelets up slightly, but Hb/red cells too low, WBC non-existent. I’ll start a daily WBC booster injection I self-administer at home.
- Due to low counts, I’m given both a blood transfusion and then a plasma transfusion before I can go home. Because there’s no other patients, Heather and I get to hang out together the whole day (usually no space for a caregiver or visitor, so she either has to stand or go find a coffee shop nearby to hang out and wait). We finally go home at 5:00 pm.
Monday April 14 (Day 15) Day Ward
- At the Day Ward again at 8:30 am for a blood draw, then a 2-3 hour wait for results. All numbers increasing - no need for any transfusions today
- The transplant team at Queen Mary Hospital has asked for a chest X-ray and an EKG in advance of the bone marrow transplant to make sure my heart and lungs are strong enough to tolerate the process. I’m taken from the Day Ward to Radiology to get both of those done at Princess Margaret.
- I have a meeting with the doctor who initially diagnosed me back in December. We discuss the results of my bone marrow sample. The TKI medication I take to suppress the Ph+ (Philadelphia Chromosome) is working, but not at the level they want to see going into a transplant. The lower the level at the molecular level, the more favorable the outcome (survival) post-transplant. We discuss alternatives to the current TKI I’m taking which is subsidized by Hong Kong Government. Other options are more effective and both my Hematology team and the Transplant team want me to swap to a better drug, but it will be more costly and I have to pay out of pocket. She asks us to make a decision by my next appointment, Thursday. (For more information about this, see our previous post here: https://www.pluckyday.co/the-price-of-life/)
- They schedule Round Five of chemotherapy for April 28 (this will eventually change, we don’t put anything in ink on our calendar) and then I get to go home at 3:00 pm.
Thursday April 17 (Day 18) Day Ward
- At the Day Ward at 8:30 am for blood draw (Hb is down which is a normal pattern, everything else is up) and to meet with the doctor to give our decision about changing to a more effective TKI medication.
- Our youngest son arrives at the hospital to join us for the doctor meeting. This is a big decision which affects the whole family. We take a deep breath and tell her we’ve decided to go with the most effective drug, which will cost us $35K HKD ($4500 USD) per month (Please consider supporting us with a paid subscription to www.pluckyday.co!)

- They postpone Round Five of chemotherapy as I will need radiation of my head, and the Radiology Department tends to be less flexible in scheduling than the Hematology Department. They don’t want me to have radiation while I’m having the post-chemo dip of all my levels, so they’ll wait to start my next round until after radiation. My initial appointment with Oncology Radiation Department is scheduled for Tuesday April 22, the first day after the Easter public holiday.
Tuesday April 22 (Day 23) Oncology Radiology Department
- We meet with the Oncology Radiation Department doctor at Princess Margaret Hospital who goes over the process of head and brain radiation, including the side effects. I’ll have eight sessions, each lasting 5-10 minutes. This will happen soon, but we’ll probably only get the start date the day before we need to show up.
Wednesday April 23 (Day 24) Day Ward
- Back at the Day Ward at 8:30 am for another blood draw to check my levels. It’s very busy in the Ward today, no available seats so Heather leaves for a coffee shop nearby. It took two hours for them to draw my blood and then I wait three hours for results. Hb and Platelets are up, Neutrophils and WBC are down, which means I’ll need to do a WBC booster injection when I get home.
- I talk with the doctor about my radiation schedule and she confirms that I’ll pick up the new TKI drug on Friday and begin taking it Saturday.
- I pick up some medication at the hospital pharmacy, Heather returns to the hospital and we head home at 3:00 pm.
And that brings us to where we are in real time.
So far, I am still technically in Round Four treatment/recovery stage. Round Five won’t be scheduled until I complete the eight days of radiation on my head/brain. This month I still have the following appointments lined up (more already scheduled for May):
Thursday April 24 (Day 25): Oncology Radiology Department planning appointment
Friday April 25 (Day 26): Oncology Radiology Department CT Scan in the morning, Pharmacy appointment to pick up new TKI drug in the afternoon.
Tuesday April 29 (Day 30): Day Ward to flush PICC line
As you can see it is a busy, relentless schedule, but I’m always happy when I can be at home at night in my own bed, eat better, and get a little bit more exercise. I work hard to build myself back up during this time, so I’ve got some strength before the next round of chemotherapy knocks me back down again.
Thank you for reading! If you’re interested in supporting us with a one time financial contribution, consider giving any amount through Buy Me A Coffee!