Michael’s Medical Journal: Brain Radiation
Last week I completed my brain radiation treatments, a total of eight sessions! I have Mixed Phenotype Acute Leukemia, so I get treatment for both Myeloid and Lymphoblastic types of cancer. We learned Lymphoblastic Leukemia cells like to gravitate into the Central Nervous System (brain and spinal fluid) and hang out there, so they do radiation as a method of prevention. After completing four rounds of chemotherapy, I was referred to the Radiotherapy Department within Princess Margaret Hospital for the next step in my treatment.
It took a little while to get an initial appointment, and even longer to schedule the treatment, as I needed eight consecutive days (not including weekends and public holidays when the Radiotherapy Department is closed). Tuesday April 22nd was my first assessment appointment, where we learned about the process, side effects, risks involved, and signed the consent forms. They emphasized this was very low dose, definitely a relief.
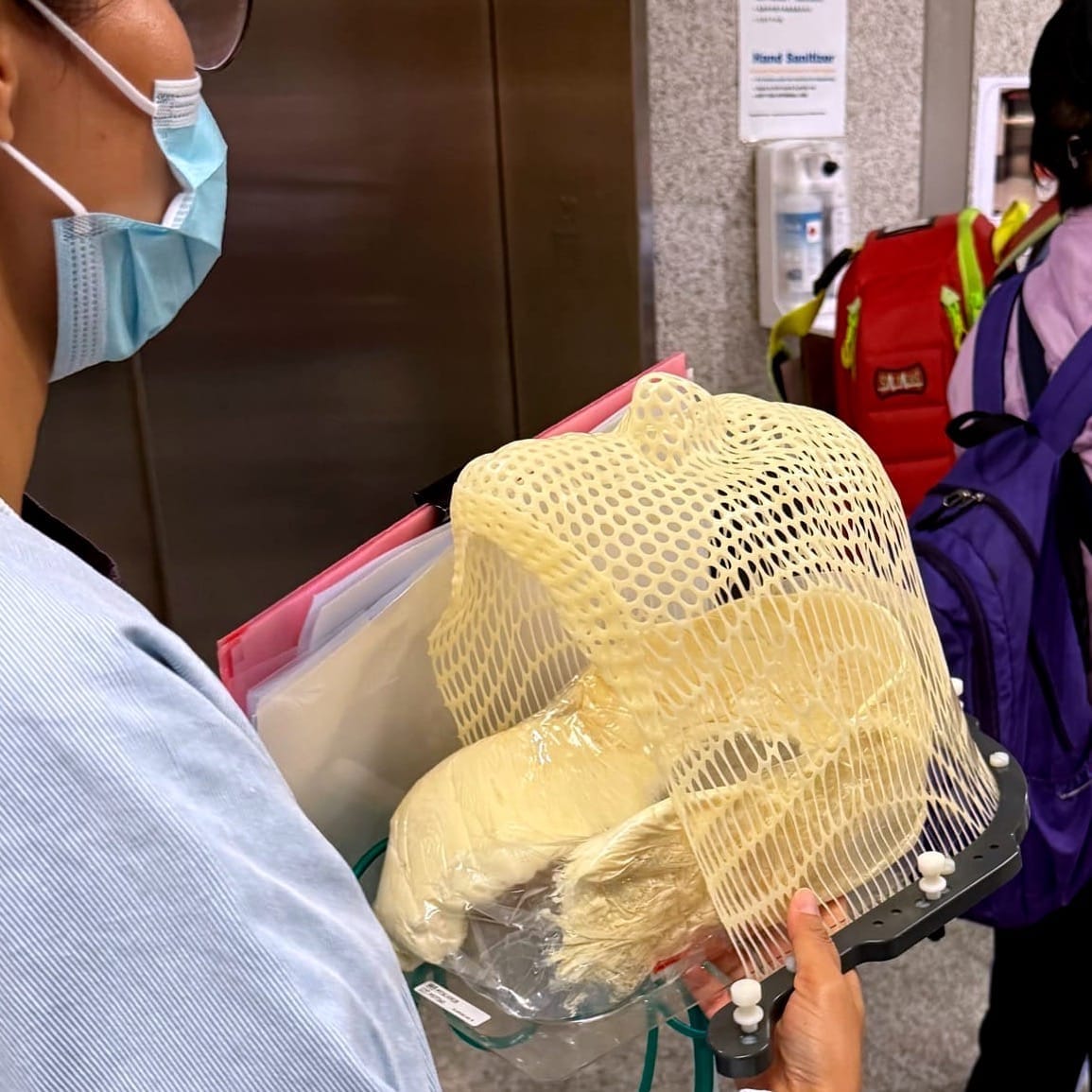
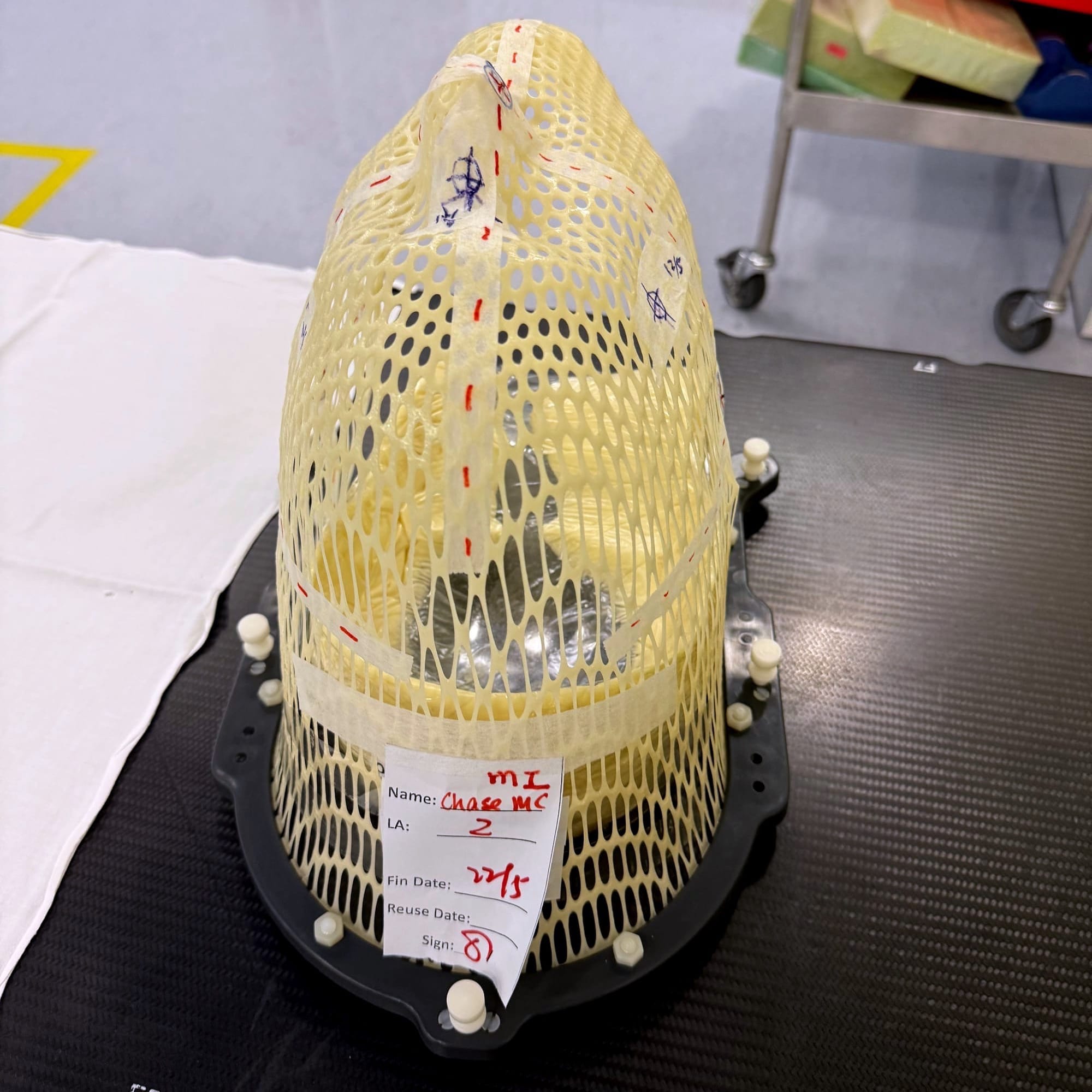
Thursday April 24th was my planning session appointment. They first made a mold of the back of my head, with extra padding for neck and head support to hold it in place. Then they placed a heated plastic mesh over my face (like a vacuum mold, without the vacuum) and pressed the mesh tightly around my nose, eyelids, chin, jawline and face. Both molds work as a clamshell around my head, then clamp to the table to assure I can’t move my head even one millimeter in any direction. It hardens as it cools, and seriously I could not move anything, even my lips or mouth. The mesh allows me to breathe through my nose, and I can barely open my eyelids to look through the mesh to see a very narrow vision of what’s happening directly in front of me.
Next they took me and my newly pressed and cooled mold to the CT scanner room. I was clamped to the table with it while they did a full scan of my head and brain. The Radiotherapy Department was then able to create a 3D map of where to precisely target the low level radiation into my head.
It took two and a half weeks to finally get scheduled for treatments. I was told two of the four radiotherapy machines were down, creating a backlog of people requiring treatments. Monday May 12th we started the first treatment, which took longer than the rest. Once they got me situated on the table, clamping my mask down to immobilize my head, they used the machine to do a 3D X-ray of my brain. This was mainly to confirm the CT scan information, in situ, with the machine, and then start the programmed radiation treatments. In total the X-ray and the radiation probably lasted a total of 15-20 minutes. During each appointment the attendants secured my head to the table, made alignment markings on my mask mold, placed a panic buzzer in my hand to use if I had any discomfort or a panic attack, then left the room, closing the large radiation-proof door behind them.
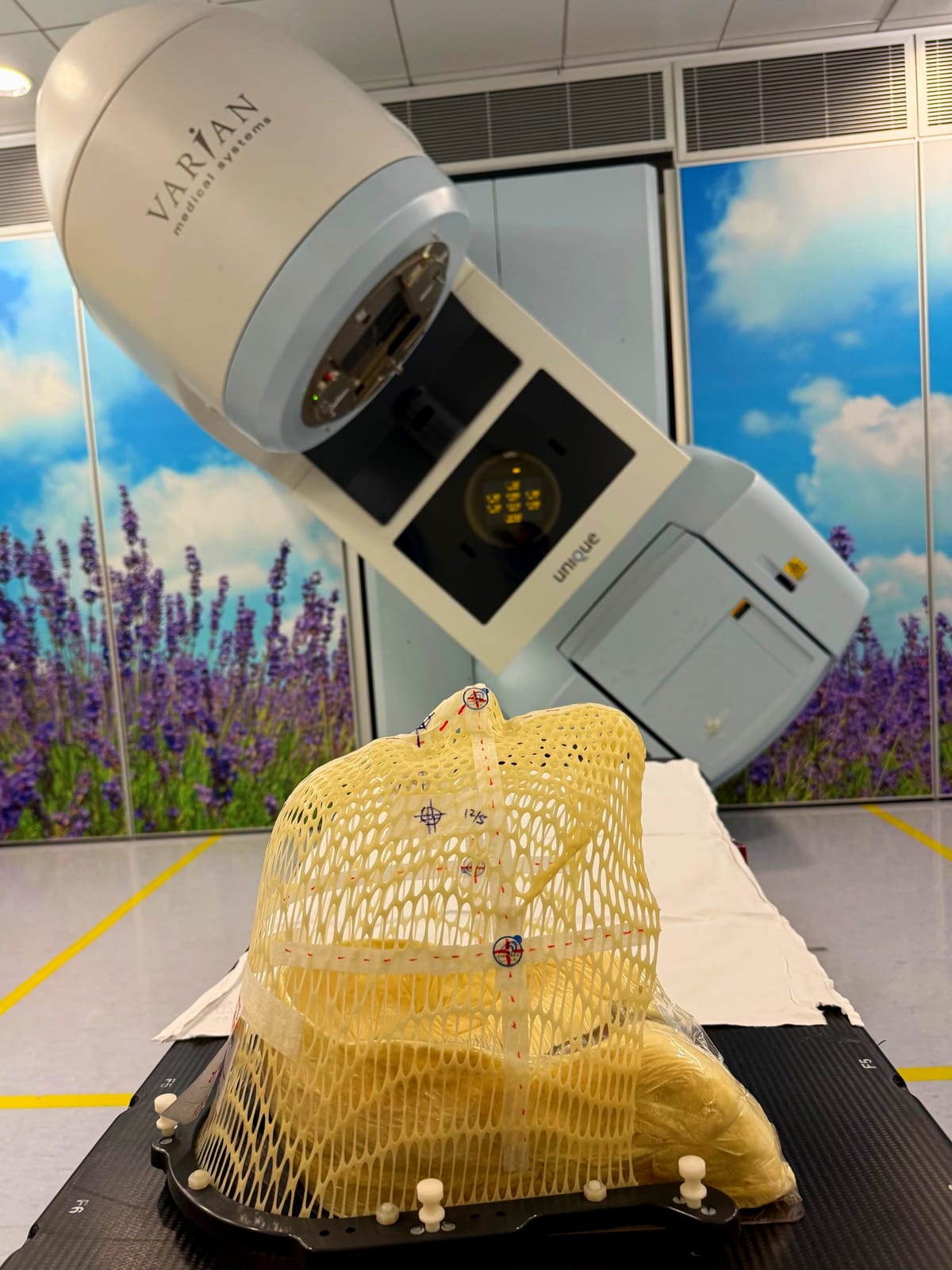
I had to practice meditation and relaxation techniques to be as calm as possible, slowly breathing in and out through my nose. The machine (pictured at the top of this post) rotates around to radiate one side of my head, then rotates to radiate the other side, and finally rotates to do one short blast in the center. With eyes tightly closed, I could see a bright purplish light through my eyelids, hear a loud buzzing sound (like a tig welder or electrical arc), and smell ozone or electrical discharge each time the radiation was applied. Once that was done, the attendants re-entered the room, removed the head mold, helped me up, and gave me my appointment card with the time for the next day’s treatment.
The next three days (Tuesday, Wednesday, and Thursday) went off without a hitch. Once they called my name, it was very fast. They confirmed my identity, asking me to repeat my full name and Hong Kong ID card number to make sure the program they’d pulled up was mine. Then they did it a second time after entering the radiation room when the attendants matched my mask and the internal display to me. The process of placing me on the table, securing me, running the radiation sequence, and exiting with my appointment card took no more than ten minutes in total. Add in the commute of forty-five minutes each way plus waiting about fifteen minutes for my name to be called, and each treatment took about two hours out of our day. Round trip the transportation cost each day was $340 HKD / $45 USD. Heather negotiated a rate with a taxi company which saved us about $120 HKD / $15 USD a day. Every little bit counts because it all adds up!
I’d been scheduled for five treatments the first week, Monday through Friday, followed by three more treatments the second week, Monday through Wednesday. But like most everything else about this journey, the plan went a bit sideways.
On Friday May 16th, in addition to the scheduled radiotherapy appointment, I had my normal weekly appointment in Princess Margaret Hospital’s Day Ward for a blood draw, a change of dressing and flushing my PICC line, a consultation with the doctor to go over the test results, and a refill of prescription medicines. Our plan was to go to the Day Ward first, have the nurses take blood and change the dressing, then while waiting the 2-3 hours for the test results, we could just pop over to the Radiotherapy Department next door for a few minutes and do my radiation. I’d be back in plenty of time to meet with the doctor to get my lab results and then pick up my meds at the pharmacy. Genius, right? Except none of that happened.
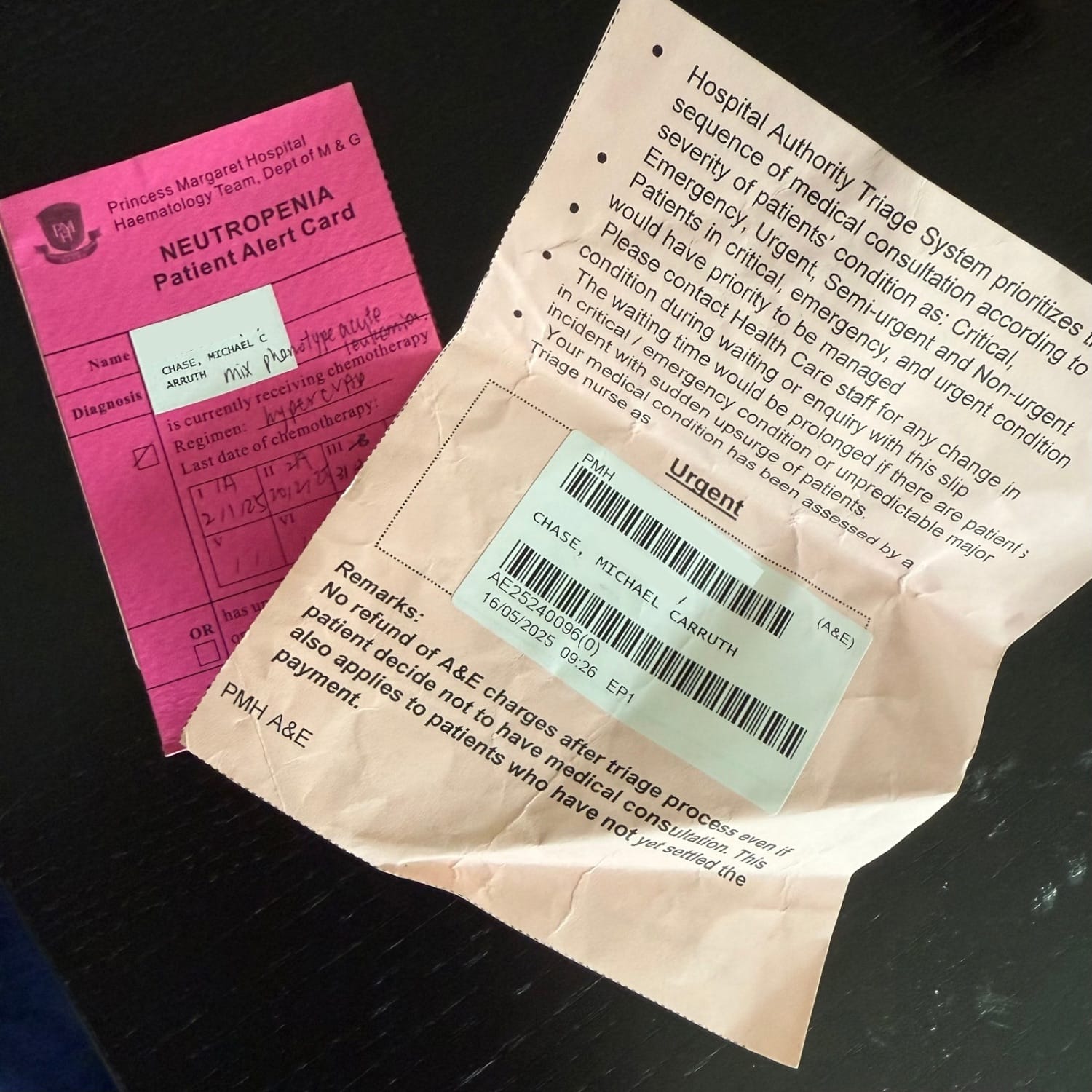
I take my temperature at home twice daily to check for fever. If my temperature hits 38C (100.4 F), I need to go immediatly to the nearest A&E (Accident and Emergency, or Emergency Room), where the protocol is to admit me to the Hematology Ward where they will begin searching for infection. I have a bright pink priority “Neutropenia Patient” fast-pass card I keep in my wallet which jumps me to the head of the line in the A&E. They take it very seriously because the leading causes of death for Leukemia patients are secondary infections. Being severely immunocompromised means we lack the ability to fight off infections, so simple things can quickly turn into deadly emergencies.
That Friday morning I’d checked my temperature at home like usual and it was normal. In the Day Ward they check each patient’s weight, blood pressure, and temperature before starting any procedure. When they checked mine, the ear thermometer registered a temperature of 38.4C. They checked it again with two other thermometers, but got a reading over 38C each time. Then they had me sit and rest in the air conditioned waiting room and drink water for a few minutes before they checked it one more time. It was still over 38C. They sent me to the next block to the A&E department so I could start the process of being admitted to the Hematology Ward upstairs. A&E took lots of blood and a chest X-ray and then an attendant walked me up to Hematology, where I was given a course of antibiotics and three day stay for monitoring.
This happened to me once before after my third round of chemotherapy in March. I’d gone to the Day Ward for a follow up visit and ended up in the hospital for five days. It is fairly traumatizing, as I felt completely fine, I didn’t have a fever when we left the house, I thought all was good. We’ll just be there a couple hours waiting on test results and then we can get on with our day. But then for a few moments my body warms up and suddenly everything is completely out of our control and I end up with a three to five day stay in the hospital, where no further symptoms ever develop. Both times this has happened my temperature has returned to normal on the one minute walk from the Day Ward to the A&E. But because it has now been registered in the system that my temperature was above the 38C threshold, the protocols are triggered. The risks are too great to ignore.
Now I’m filled with anxiety each time I arrive at the Day Ward to get my temperature taken. A nurse coming at me with a thermometer has become a triggering event. Since I have to go through this weekly, the fear is palpable.
During this second time of having a fever, going to A&E, being admitted, and then missing my Radiotherapy Department appointment I was furiously angry and depressed. Was this going the be the rest of my life? Not being in control, worrying over every minor symptom or fever, disrupting my life for days each time it comes up? The complete lack of control, interruption of life and comfort of being home was just honestly depressing and put my head emotionally in a really dark, dark place.

The fever came back and persisted Friday and Saturday night, but finally relented on Sunday. I was given three injections of heavy antibiotics each day. They finally discharged me on Monday, allowing me to go back to the Radiotherapy Department to continue my radiation treatments. They extended my treatment through Thursday, adding a day to make up for the missed day on Friday.
The rest of my radiation appointments went off without a hitch. On the last day, they let me take a picture of my mask before sending it out to be destroyed. They don’t allow patients to keep them here, though we have friends in other countries who were given the option to take them home. I don’t think I would have wanted to, but I am glad I was allowed to take a photo.
Just a note: I completed my most recent round of chemotherapy on April 7th, and have been home since April 8th. Until the radiotherapy started, I’d only been coming into the Day Ward once a week for blood draws and checkups with the doctor. This has been the longest time at home since I started this journey back in December. Excluding the three days in the hospital due to fever, I’ve been home for seven weeks!
Now that my head radiation is complete, it feels like we’re at the end of the opening act of my treatment plan. We’re preparing for my upcoming bone marrow transplant (all details still TBD), which seems like the main event. A new location, a different cast of characters, and all new drama, suspense, and intrigue. Stay tuned for more information coming soon!
Enjoy what you’ve read and want to help fund more of this content? Consider sponsoring our efforts through Buy Me A Coffee. The money goes toward a less caffeinated but still necessary taxi ride to the hospital for treatments. Thank you for your support and we hope you have a Plucky Day!