Michael’s Medical Journal: Diagnosis and Round One of Chemotherapy
Information = Knowledge = Understanding. Tracking my stats gives me a small sense of control in a very uncontrollable situation!

With the never ending uncertainty, constant changes, and new information coming at us daily, I’ve found tracking and monitoring my own stats helps me to understand and feel slightly more in control (information = knowledge = understanding). It also makes me more aware of what my body is doing so I can anticipate what’s coming or understand why I feel as bad as I do. This is a recap of late December and January lab results, findings, and my treatment plan. Hopefully this gives you some insight on what we’re monitoring and discovering as part of this journey.
During the Diagnosis Phase, I had constant blood draws and lab tests. My White Blood Cells were off the charts to begin with, due to the Philadelphia Chromosome (Ph+) mutation, over-producing immature blast cells at an alarming rate. Normally White Blood Cell count should be between 4 and 11, but mine were between 80-100 at the time I was admitted to the hospital. This was a terrifying period when I needed to learn a whole bunch of medical stuff I never previously wanted or needed to learn.
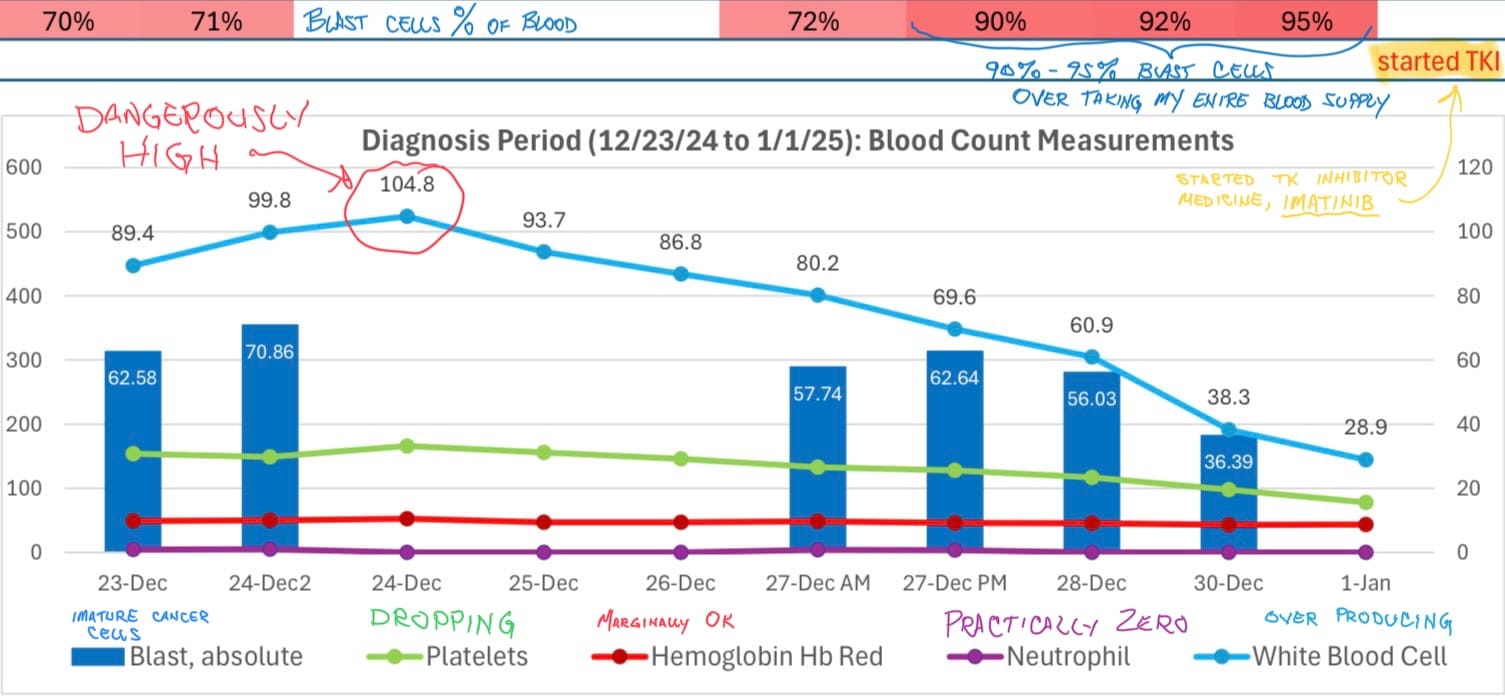
On New Year’s Day, I started taking Imatinib (a Tyrosine Kinase Inhibitor, or TKI), a medication to suppress the mutated chromosome from overproducing immature blood cells. Before I began taking it, you can see at the top of the chart above my blast cells were at 95%, nearly taking over my entire blood supply.
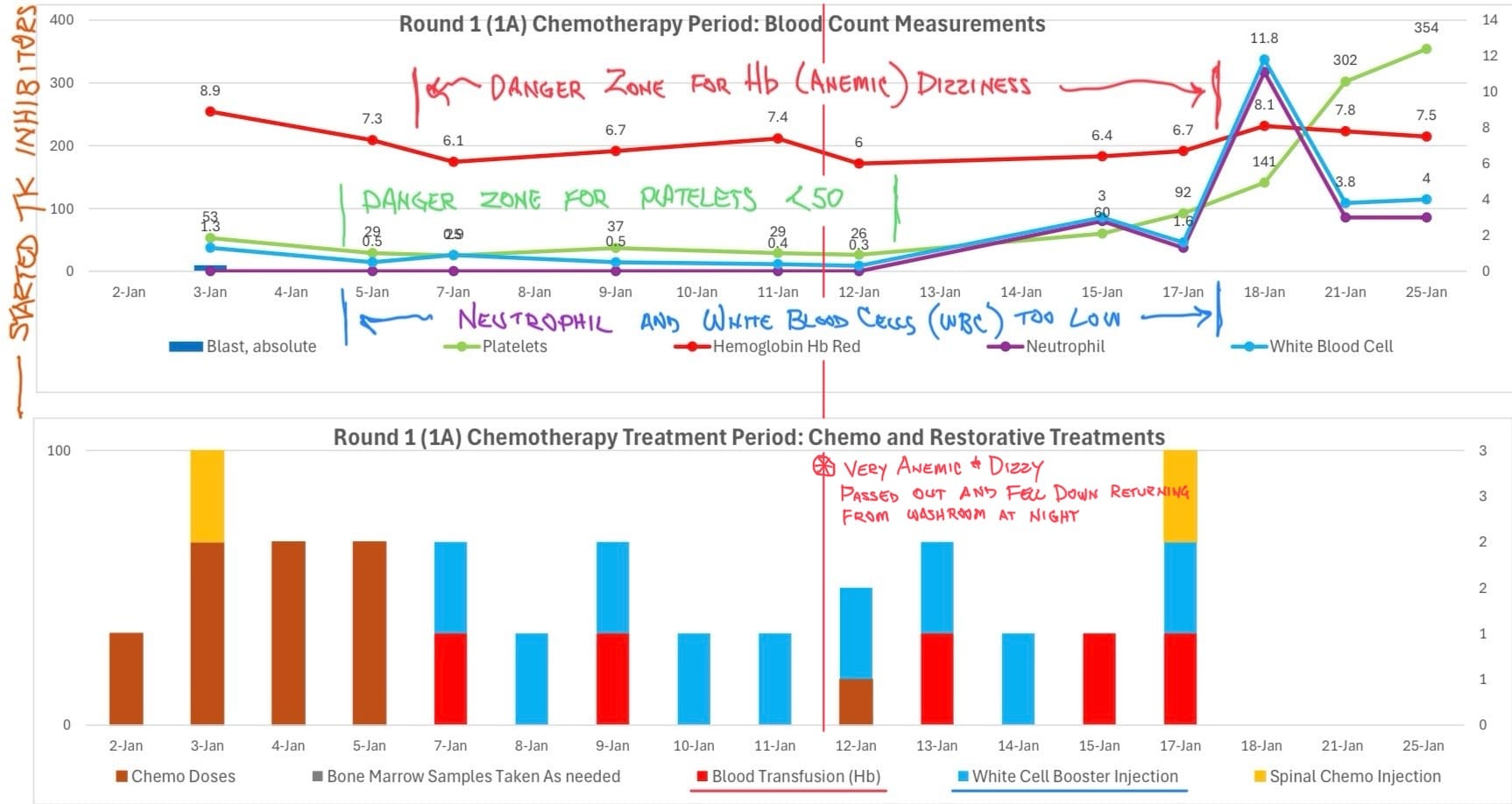
On January 2nd I began chemotherapy. You can see my Red Blood Cells (or Hemoglobin, Hb) and Platelets dropping shortly after starting. Red Blood Cells deliver oxygen to your body, and a lack of them will result in anemia. The danger zone is anything under 7. I found this out the hard way.
My Hb dipped below 7 on January 6th and kept hovering in that range. I had been feeling dizzy and weak, but I thought if I went slowly and hugged the wall on my short walks to the bathroom, just 6 meters (or 20 feet) away, I would have it all under control. But close to midnight on January 12th, I went to use the facilities, and on the way back I blacked out and fell on my face, landing on a couple rolling IV stands and blood pressure monitor legs. My roommates were awake and witnessed the fall, and started shouting for the nurses. They came quickly and helped me get back into my bed, and inspected me for cuts, bruises, or abrasions.
A fall is important to inspect, because my Platelets (which help blood to clot) were also at a dangerously low count of 26 (normal is 150 - 400). This meant I could have internal bleeding or not heal from a cut or contusion. After my fall, the hospital staff immediately took me for X-rays and a CT scan, to make certain I had no brain bleed or other internal injury. I called Heather in the middle of the night while I was crying and scared her pretty badly.
The inability to really understand how weak my body was, how dizzy, or how just standing up from the bed would get my heart rate pumping and my blood pressure elevated, made me incredibly fearful. The first round of chemo was a steep learning curve for all of this.

As we monitor my blood levels, part of the treatment plan includes transfusions of blood, plasma, or WBC booster injections when my numbers get too low. This may happen while I’m admitted to the hospital, or after discharge, during a weekly checkup at the Day Ward.
- If my Hemoglobin (Hb) Red Blood Cells get below 7.0, I will get a blood transfusion. I needed five transfusions during Round One of chemotherapy. The first time I had a blood transfusion (after my fall incident), it felt like a shot of espresso. It was amazing how I went from very low energy and fatigue, to being animated and talking with energy within a 30 minute timeframe.
- If my Platelets get below 50, I will need a plasma transfusion (I recently needed two plasma transfusions after Round Four of chemotherapy).
- If my White Blood Cells or Neutrophil counts are too low (below 4.5 or 2.5 respectively), I will need a booster injection to jumpstart the production of white cells again (during Round One, I needed nine booster injections). If anyone has needed insulin shots before, it’s basically the same thing — a shot in the abdomen with a retractible needle. I eventually learned how to self-administer the shots to take them at home during my home recovery periods between rounds.
Whenever I have a blood test, I always ask for the results of these four main indicators: Hemoglobin (Hb), Platelets, Neutrophil, and White Blood Cells. Those indicators will give me an understanding of where my body is in the recovery or treatment cycle and what corrective steps the doctors will likely choose to get me on track to better health. It’s a small thing, but it helps me feel like I’m a participant of the process, and allows me to speak with knowledge about the status of my health. It also gives me just an ounce of feeling like I have some control over this very uncontrollable situation.
Thank you for reading! If you’re interested in supporting us with a one time financial contribution, consider giving any amount through Buy Me A Coffee!