Raining. Pouring. Flooding.
Once again feeling like we can’t catch a break.

Do you recall the end of the last post where we were celebrating 100 days post-transplant? When Michael mentioned some pain he was having, and how we might need to head back to A&E (E.R.) to get that checked out because a typhoon was on the way? It was a couple weeks ago but we’ve lived what feels like many months since then.
Having spent more of 2025 in the hospital than out of it, Michael is understandably wary of going in unless it’s absolutely necessary. But due to the heightened emotions surrounding hospitalization, we are terrible judges of what is absolutely necessary. Nothing is ever quick or uncomplicated with his health. Thankfully we have a handy spreadsheet of all the reasons we need to report to A&E. In this case, other than the significant pain and some gastrointestinal issues, Michael was just ever so slightly beneath the threshold in the list of reasons requiring an emergency trip.
We delayed going in on Friday night, and then dragged our feet all day Saturday. Ultimately we did take Michael to Princess Margaret Hospital that Saturday evening, primarily due to the rising typhoon warning… we didn’t want to get stuck at home, or put our local ambulance crew at risk if the storm got worse. Before we left the house, we packed a bag for Michael with items he would need should they admit him. It was wise, because of course, they did admit him. Instead of the General Ward, they found him a bed in Hematology where he was greeted with warmth and enthusiasm by the nursing team who walked with him through chemotherapy during the first half of the year.
Throughout Saturday night into the early hours of Sunday they ran several tests on Michael. The culprit behind the pain? An angry, inflamed gallbladder, which was brewing a little infection. The Princess Margaret team consulted with Michael’s transplant team at Queen Mary Hospital, and together it was decided the risks of surgery to remove Michael’s gallbladder were lower than the risks of the infection (and potential future issues) from leaving it in. So he signed stacks of paperwork, I ran in to visit him for one hour, and then he was whisked away for surgery.
In the evening I went back for visiting hour and had the actual fright of my life to find there was someone else in the bed Michael had occupied that morning, where all his personal items had been just hours before. No one had called me to say there’d been a problem with surgery and my mind went to the darkest place. I tried to steady myself to walk to the nursing station just as my phone rang — it was the nurse at the nursing station. The Hematology Ward could not keep him because he needed more personal, specific post-surgical care than they were equipped to provide. They asked me to pack up his stuff (which had simply been moved to another bed, whew) and take it to the next block where he’d be transported shortly. I was so relieved he was okay!
The week in the special care surgical ward was awful.
The turnover was rapid, with most other patients there just one night before being discharged. The Hematology Ward has three beds to a room with privacy curtains between each bed, and the transplant ward was a single isolation room and private bathroom. The surgical ward has eight beds with curtains pulled all the way open for the staff to have full view of each patient. We absolutely panicked, and not about the loss of privacy and space or the chaos and noise. It was going from our tidy, cozy home with all the air purifiers running, the cleaning schedule of all soft goods to keep risk of infection down, the daily showers and sterilizing of Michael’s Hickman Line, and constant best practices for Michael’s health including limiting the number of people around him, to the Wild West of a huge ward with dozens of new people in and out every hour, no shower at all for the whole week, no control over anything other than our attitudes. We prayed for supernatural protection from everything around him.
It didn’t help that the whole week felt a bit like the movie Inception, where as soon as the world realizes you are an intruder, it starts fighting back against you. Princess Margaret Hospital is much closer to our home than Queen Mary, but even on the days when I left over an hour early, I would still get there late, due to unexpected traffic, road works, accidents, or car trouble. It was exhausting to go back to making two trips a day to bring Michael (edible) neutropenic-safe food during the very strict (and brief) visiting sessions. Being in a ward where there was so much pain and struggle on full display was emotionally draining. I was thrilled when they said Michael could go home on a Friday night, seven days after we’d first brought him in.
There was no time to catch our breath.
On the Friday he was released, Michael developed what looked like a blood blister on his left hand. It didn’t hurt or itch. On Saturday there were a few red bumps on his left arm. By Sunday morning the red bumps turned into blisters. Sunday evening they had doubled, but were limited to his left arm and hand. To me, it looked like Chicken Pox. Once again we had to decide if this was one of those “absolutely necessary” events requiring a trip to A&E. Once again Michael was shaking at the thought of going back after having just been in the hospital for a week. Once again Michael packed his bag with the items he would need if he was admitted.
Since rashes of any kind can be a sign of his Graft Vs Host Disease, we decided we’d better take him all the way to Queen Mary Hospital’s A&E so he could be under the same roof as his transplant team. Exhausted and unenthusiastic about the situation, we decided to let Michael get one more night of sleep at home and head into Queen Mary first thing in the morning.
Michael has a little pink “fast pass” card which allows him to jump the queue at the emergency room and we have saved at least a full day of waiting this year thanks to the “privilege” of being a cancer/transplant patient. We went immediately to triage, were told to wait a moment, and then were summoned back to see a doctor before we could even warm the waiting room seats. The doctor took one look at Michael’s arm and said, “Oh that’s Shingles. You’re a transplant patient and immunocompromised? Yeah, we’ll need to admit you. Likely for about a week.” Not unexpected, but still disappointing. They told us to head to radiology for a quick chest x-ray and then have a seat until they called Michael back again. This time the wait was about 15 minutes.
They called Michael’s name and we saw a completely different doctor, who said, no, he didn’t need to be admitted, they would just prescribe some antiviral pills and cream and send him home. Hooray! We pointed out that Michael had been scheduled to have his stitches from the gallbladder surgery removed that day, over at North Lantau Hospital which is the closest to our home, and asked if it would be possible to get it done then and there so we didn’t have to drag Michael to yet another hospital. They said sure, but we’d have to wait a little longer since it wasn’t an emergency.
An hour later we were summoned to a procedure room where a nurse carefully removed Michael’s stitches, showing me how to take care of the incisions. As someone who has had many, many incisions and stitches in my life and as the mother of two sons who have needed to be stitched back together with some regularity, I already knew how to take care of them like a pro. However, I am almost never included in any of the conversations about Michael’s care, as they never happen during visiting hours. So believe me when I say I lapped up her kind instructions like a starving puppy, just thrilled to be in the room for once.
Side note: the A&E nurse, though trained in doing so, never gets to take stitches out because people usually only go to the A&E to get them in. It was a treat for her to be on the other side of the process for once!
At home, Michael started the antiviral meds and we felt grateful, first for being able to come home, and second because surely things would start getting better now.
Of course, things did not get better, they got worse.
The blistery Shingles rash got bigger, with blisters growing and combining with nearby neighbors creating giant yellow and pink bubbles filled with very contagious goo. Contagious, that is, to anyone who has never had Chicken Pox or the Chicken Pox vaccine, who will likely develop it if they come into contact with someone who has Shingles. Shingles itself you get from yourself… it can develop later in life in anyone who previously had Chicken Pox, as the virus lays dormant in the nerve cells near the brain in the spinal cord. It commonly pops up during times of stress or when the immune system weakens, such as in a transplant patient who is on a buffet of immunosuppressant medications to keep the Graft vs Host Disease at bay.
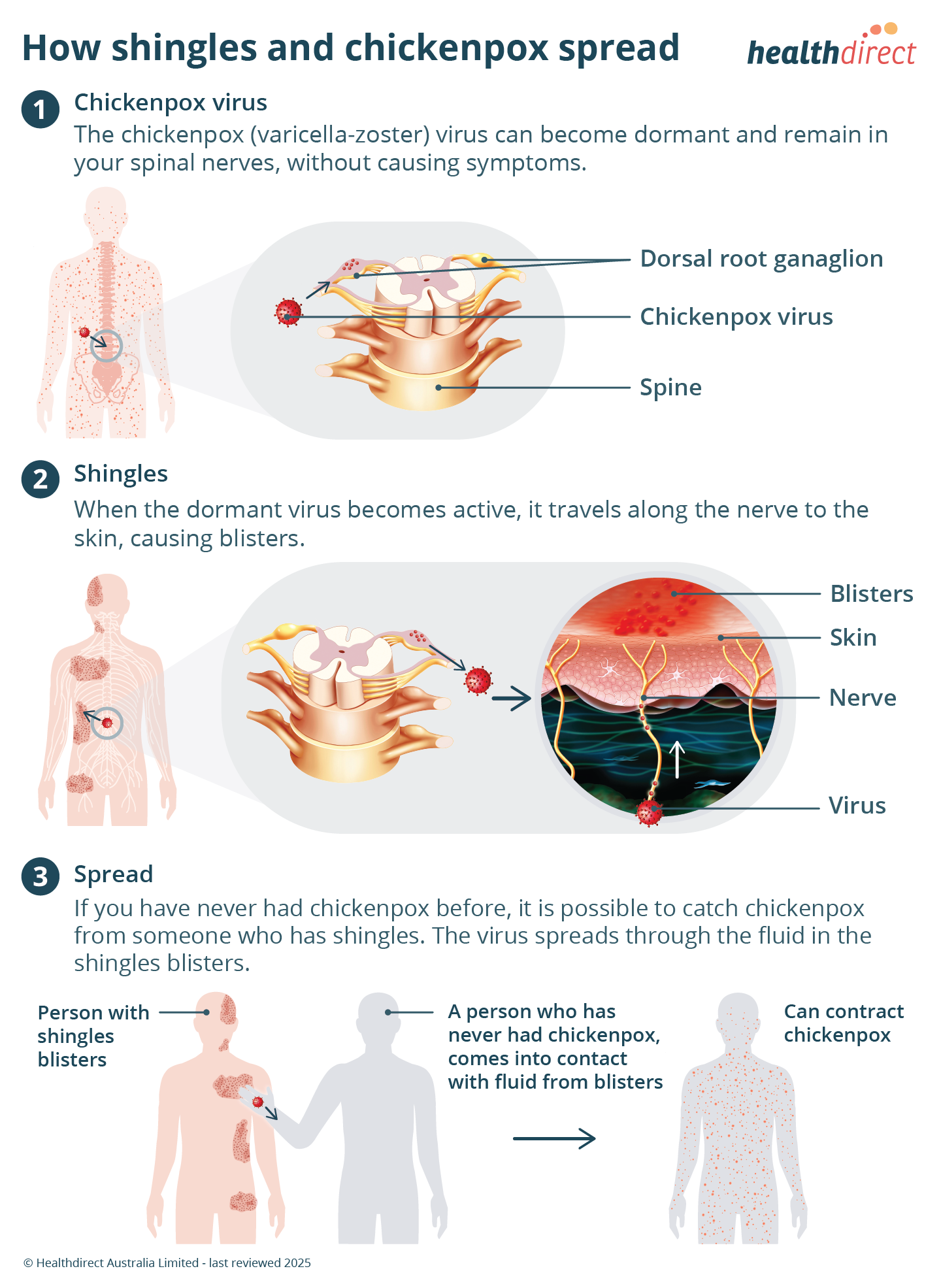
Turns out that even though Michael didn’t show up to class or read the textbook, he is acing the test. 20-30% of stem cell transplant patients who have had Chicken Pox get Shingles around the three month mark, post-transplant. Michael’s first blister appeared three and half months after the transplant, right on (diabolical) schedule.
We watched as the blisters increased in size and number on Monday, Tuesday, and Wednesday. By Wednesday evening Michael was experiencing substantial pain. He had a blood draw appointment and doctor visit scheduled in the Transplant Out-Patient Clinic at Queen Mary Hospital for Thursday, so we were holding on for that, prepared to ask if there was a stronger antiviral and pain medication that Michael could take.
Thursday morning when they took Michael’s blood, he showed the nurse his growing blistery rash. The nurse told him he could not stay in that ward, or even on that floor, because everyone there is like Michael, severely immunocompromised, and Chicken Pox isn’t as ubiquitous in Hong Kong as it is in America. She said he would need to go somewhere else to wait and that as soon as the doctor had seen all the other patients for the day, they would call Michael on the phone to come back up and see the doctor. In Michael’s weakened and painful state, there weren’t many options of places to hang out for what would ultimately turn out to be five hours. The commute to the hospital from our home is over an hour, so it wasn’t going to work to just go home. Ultimately we found a quiet, isolated corner in the hospital’s Pacific Coffee, but it was far from ideal, sitting up in a chair for so long, just a few weeks out from major surgery and in so much pain from the Shingles.
When we were finally called back up to meet with the doctor, she took one look at growing rash, audibly gasped, asked how many days he’d been on the oral antivirals. Four days should have seen marked improvement, but it was only spreading. She said the oral meds weren’t enough, he definitely needed to be admitted for IV medications, including immunoglobulin, stronger antivirals, and more targeted pain killers. He would be placed in the medical isolation ward. We were asked to sit in the hallway as far away from anyone else as we could get, and then waited on the paperwork for admission. We cried, again. I guess it’s our tradition at this point.
The nurse came out to tell us that there was no space in the isolation ward, so they would put him in the general medical ward until an isolation room opened.
Having just been discharged from the general surgical ward at Princess Margaret a week before, our context for “general” wards meant a huge lack of privacy, the revolving door of visitors coughing and sneezing, and fellow patients in misery following their surgical procedures. We didn’t feel brave or plucky about this at all.
Up we went to the general medical ward, pressing the doorbell since it was not visiting hour, and walked in to find the head nurse. I took no photos (it would grossly violate any shred of privacy everyone there deserves, not to mention something I will ever look back on with a desire to remember), but imagine a large, long space with about fifteen rows of beds, five across, no curtains, with every patient hooked up to a variety of monitors and machines. The cacophony of sound was unsettling. The suffering was overwhelming and my tender heart squeezed at the thought of spending the next week or so coming and going past all these precious humans fighting for survival. It was so beyond all our other experiences this year in size and scope of suffering.
They placed Michael in a side room which had space for four beds, but one bed had been removed. They pushed his bed as far against the window as they could, away from the door and the other two patients, and then pulled a curtain across, the sole patient in the entire ward with a modicum of privacy. It was the best possible set up in a brutally less-than-awesome situation. The doctor said they would still be waiting for an opening in the isolation ward, but for now they asked that Michael keep his mask on at all times unless he was eating and to remain in his area.
The possibility of infection went both ways… Michael with his Shingles was a risk to everyone on the ward with their varying states of medical vulnerability and lack of history of Chicken Pox. But all the many diseases represented in the other patients were a risk to Michael in his severely immunocompromised state, lacking the ability to fight off anything further. This was really the first time we saw what being “immunocompromised” meant in action. We have many friends and family members who have had Shingles, and all shared how they got antiviral meds which helped pretty quickly. In Michael’s case he may as well have been taking a placebo considering how fast it continued to spread and grow even days after he’d started the meds!
The doctors and nurses all had the same message for us: the ward had patients with pneumonia, Covid, RSV, influenza and other similar infections which weren’t safe for Michael to be around. If you’ve been following along for any amount of time, you know we don’t take public transit with Michael, go anywhere crowded with or without him, or even have visitors in our home, all in an effort to protect him from things he cannot fight. This was a bit of a nightmare, which every doctor and nurse in that ward acknowledged. We hoped and prayed for a room in the isolation ward to open up, while also praying once again for supernatural protection from anything harmful.
The next day Michael felt better. The immunoglobulin was doing the work his immune system could not, and the much improved pain management available through his IV made everything more tolerable. It would take awhile to get in the clear, but this was finally a step toward making a difference in this fight against the shingles virus.
While Michael was on an upswing, I was not doing so well.
I visited him just once a day as Queen Mary Hospital is a bit of a hike (in terms of distance, time, and cost of transit) from our home. I brought him food and small items to supplement what the hospital was providing, and it gave us precious time to be in each other’s grounding presence. But the cumulative toll of a week at Princess Margaret and now another week at Queen Mary was coming due and I had nothing left with which to pay, being physically and emotionally exhausted.
Sunday morning I woke up crying. Just went immediately from sleep to gasping for air with tears pooling on my pillow. I felt defeated and depleted and I grabbed my phone to video call Michael from my horizontal position in bed. I just need to stay home this morning, I told him, I can’t do this today, it’s all too much. We agreed I would just rest, and rest some more, and come in for the evening visiting hour instead. I finally got out of bed to climb onto the couch to watch our church streaming live from the same island where Michael is currently staying. Ironically, the message was on living your faith publicly, and I’ll be very honest here… I groaned at how public our journey has been this year and how deeply I have NOT wanted to write a post for Plucky Day to say, Oh hey friends, things are really bad (again, still, persistently, never-ending, etc.) but the good news is we are still hanging in there, having faith that our prayers, and yours, will be answered and somehow, miraculously, this story is going to have a happy ending that we simply can’t imagine from our present place on this perilous journey.
I didn’t have time to write anything anyway, because before the livestream of the service was over, I got a video call from Michael, and this time he was the one who had tears streaming down his face. He immediately handed his phone to a doctor, who told me a room in the isolation ward had opened up and they’d be transferring Michael over as soon as possible. Good news, right? Except the isolation ward he’d be sent to is a step up from the transplant isolation ward. And unlike his ten weeks over there, where immediate family could join him one at a time, no visitors would be allowed this time. I looked at the clock and realized the morning visiting session was almost over, there’d be no time for me to run over for one last hug. There would be no seeing him in person for up to a week.
The doctor said we were free to decline, but she mentioned the same thing all the other doctors had said: everyone else in that ward, both in Michael’s room and outside the door, was very sick. Michael was already at such a high risk with the virus he was battling, why would we invite additional strain, especially while on the many types of immunosuppressive drugs he’s taking? Of course we wouldn’t decline, I told her, we would manage. Michael would go into isolation until they could get the shingles under control and complete the course of IV antivirals and immunoglobulin. But my gosh did I ever feel sad and sorry, immediately beating myself up for not going in that morning to see him.
She said that while I couldn’t see him, I would be able to drop items off for Michael at the door of the Infectious Disease isolation ward, so I got dressed and packed up about five days worth of canned fruit, high protein/high calorie supplement drinks, individual boxes of breakfast cereal, little cartons of oat milk, and plenty of socks and underwear. I was used to bringing only what he’d need for one day, as there is only the tiniest bit of storage in the general ward, and it’s not secure at all.
I made the hour-plus trek to Queen Mary Hospital and had a seat in the Pacific Coffee where I’d just sat with Michael for five hours, four days before. He was still in the general medical ward, he hadn’t yet been moved to isolation. I could technically still have the chance to see him… but the (strictly enforced) evening visiting hour had not yet started. I was an hour early. For forty minutes I prayed that I could at least see him for just a minute, that his transfer would continue to be delayed for a little while longer.
Twenty minutes before the start of visiting hour, I moved up to the second floor, standing right outside his ward. If they moved him, I would be able to hold his hand for the ride in the elevator from the second to the sixth floor. It would be worth it. But right after I got in place, Michael texted to say a nurse was coming to let me in because they were about to move him and he’d asked if I could help pack him up since once of his hands is covered in painful blisters. So in I went! And then as soon as I got there, someone brought his dinner. The nurse said he should eat first, then they’d move him. My hope had been to have just one minute in a lift with him, but I got a full hour sitting on a hospital bed with him! Glorious!
All too soon it was time to accompany him upstairs, only as far as the barrier outside the doors to the Medical Infectious Disease isolation ward. A sign at the door reminded all who passed that no visitors were allowed in. Finally a closed door that I couldn’t just wave my hand in front of the motion detector and have it open.

In trying to find a way to spin this situation positively, I decided that though it would be extremely hard to not see my Beloved in person for many days, I was being given the gift of staying at home and resting. I would take it. Surely nothing else could possibly go wrong, right? Right??
We are in the middle of a two year lease on our home.
In Hong Kong, the standard rental agreement is for two years, the first year is fixed and you can only get out of it by paying the remainder of the year or finding someone else to take over your lease. The second year either party (owner or tenant) is allowed to give two months notice to vacate. The owners of our flat left Hong Kong during Covid and are getting close to retirement. The country they live in taxes them heavily for having two homes, and they have become very anxious to rid themselves of this second home in a country they don’t intend to live in again.
Our flat, while smallish by American standards, is huge for Hong Kong. It’s actually two smaller flats with the middle wall removed and some remodeling to make just one kitchen instead of two. Both our adult sons still live with us (we’ve raised them for most of their lives in Asia, families remaining together under one roof is the way, and right now with Michael’s health it’s the largest bonus ever) and the way our home is laid out, they are at one end and Michael and I are at the other. For the first time in their lives, the boys aren’t sharing a room. It has a large central living area with our sofa and a huge dining table where in the time before cancer we’d comfortably and regularly seat ten people for dinner and deep conversation. We’ve lived in this home for three years and we love it so much. Having signed a second two year lease, we were pretty grateful that no matter what happens with Michael’s health, we have a place to stay that is peaceful and spacious (to us). The walls are filled with art, color, and texture, surrounding us with beautiful reminders of the people and places we love so dearly.
The real estate agent, who also acts as a property manager on behalf of the owners, had informed us that they were interested in selling when we moved in. But she also said it is very hard to sell these double units because while they are combined thanks to the missing wall, they are still two individual units for tax purposes. We get two gas, electric, and water bills, and two sets of dues owed to the management company. She also told us that the owners were specifically seeking investment buyers, who would purchase this place with tenancy already secured. For over two years we heard nothing at all about any potential sale, so we put it completely out of our minds. And then, right at the beginning of this year, when we were still reeling with Michael’s diagnosis and trying to grasp the long road ahead of us, the agent showed our flat a few times. I knew that while the first year was pretty secure even if it sold, starting October 15th a new owner (or even the current owner) would have the right to ask us to vacate with two months notice. Which would be right before Christmas, the one year mark of Michael’s diagnosis. No time is a good time to move, but over the holidays is certainly one of the worst.
Nothing came of it, but in the midst of praying big, audacious prayers for Michael to make it through this awful health challenge and for our family to remain intact through it all, I also began to pray that somehow God would just give us this home. That we wouldn’t have to move for a long, long time, that we would finally have a permanent address in Hong Kong, which will be our home for the foreseeable future due to Michael’s care here. That our kids, who are just at the start of their careers, will have a place to stay as long as they want. That once we come out the other side of this, our huge dining room table will once again be regularly filled with guests for dinner and deep conversation.
Big and audacious doesn’t even come close to what it means to ask for this, but I have never stopped asking.
This week, in the middle of everything else going on, on the very day I woke up crying and then Michael was moved to the isolation ward, the agent once again contacted us. Perfect timing, I thought, dripping sarcasm. October 15th, that date which had seemed so far away back in January was suddenly in the rear view mirror. And the owners are now pressuring her to sell this place ASAP. If not to an investor who will buy it with tenancy in place, to someone who wants to buy it for their own use, which they can do by giving us two months notice.
Instead of truly having these days of separation from Michael to rest, they have been filled with appointments of potential new owners coming by to look in every room and cupboard and imagine their own belongings here. In addition to feeling defeated and depleted, there’s a bit of demoralization creeping in as well, as each new person stops by (all in masks at my request), potentially steering what happens to us next. There is no part of my very vivid and creative imagination that can figure out how we would be able to move and keep Michael both safe and uninvolved in the packing and unpacking required, or for there to be some unknown store of energy I haven’t yet tapped into which would get me out of bed and focused on dramatically downsizing without spiraling into the anxiety and depression which is forever lingering just out of view.
What I do know is this: on the day we had to decide whether or not to “upgrade” to the better (expensive) medication which might give Michael a better chance at life, I sat down with both my sons and laid out all the negative and difficult possibilities I could think of which might come from a choice to say yes. One of them was losing our home, of having to proactively move into a much smaller place, especially if Michael could not come to an arrangement to work from home as his paid sick leave dwindled. We all committed to the idea of doing whatever it takes. There was no hesitation, any sacrifice we might be called upon to perform would be worth Michael’s life, many times over.
Between the first expensive medication and the second expensive new drug added after the transplant to combat the severe Graft vs Host Disease Michael experienced, our monthly cost in medication alone is almost as much as what we pay in rent each month, in a city which has the highest housing costs in the world. Last week, right before she told us Michael needed to be admitted, the transplant doctor reminded us we should expect for him to be taking both of them for about two years. It’s a blinding sum of money, but thanks to subscriptions here, contributions through Buy Me A Coffee, and direct bank transfers, we are not sinking into a hole of debt at all. But even if we still had a reserve of money that hasn’t already gone to medical expenses, we wouldn’t be able to buy this place by ourselves right now. In the last 24 hours I had the chance to talk to the boys alone once again, just to make sure we were all still on board and deeply committed with the whole whatever it takes, and both of my sons had the same response... Of course we are, Mom.
The temptation to completely freak out right now is so huge. It would not take much. I already feel like I’m drowning and this other thing is so big and threatening. Like Michael’s immune system, my mental health is vulnerable, having gone through so much this year, with no end in sight from our limited vantage point. But here’s me, living my faith publicly and just saying this situation is beyond and bigger than me. It’s all completely out of my control, I have no contribution to make within my own power that will keep us here despite all of us deeply longing to stay. My big, audacious prayer remains that somehow God will give us this home, that we can all remain here together, that a move (and all that a move entails) is not in our future for a long while, and that our peaceful, colorful home becomes a place of deep healing, physically and mentally, for each of us on this awful journey. Wouldn’t that be awesome? I would love to tell you that story!
As the latest potential buyer visited today and I had to explain to the agent that Michael wasn’t here because he’s been admitted to the hospital yet again, I realized a long update was quite overdue and sat down to share this latest chapter with you.
So many of you are so faithful to keep checking in on us, especially when we go silent for a longer period than expected. And this was a really long period, which just seemed to keep getting worse, which made us reluctant to share. I desperately wish I had nothing but good news. My friend Carolyne (who I wrote about here) recently told me that if someone later picks up the inevitable memoir which will surely come out of this situation, no one who hasn’t been reading along in real time will believe it’s real. I have to agree. I’m living this and barely believe it’s real.
Michael remains in the Infectious Disease isolation ward for now. He needs to complete a week of the IV medications while they carefully monitor his growing blisters to make sure there is no secondary bacterial skin infection brewing. I can’t say with certainty when he’ll be home, but we know it will be a good day for all of us.
And speaking of good days — in an effort to notice and celebrate when good things happen, allow me to end this on a happy note. Benjamin, our younger son who was Michael’s donor, is currently in the middle of a much needed holiday before the busiest time of the year for him, Christmas. Ben travelled to Osaka to stay a week with our own frequent houseguest Rhett (we call our dining room The Rhett Room in his honor), and is now currently in Shanghai staying a week with our friend Ruby, who was part of our Disney Coronavirus Quarantine Club bubble, safely coming round for food and a movie each month (week?) when Hong Kong was closed up tight and we were all climbing the walls, hungry for community and connection. I’m thrilled how in this midst of all we are going through, Ben is enjoying a few weeks away from the relentless difficulty which surrounds us. I hope and pray he returns refreshed and relaxed, inspired and ready to face whatever comes next.
As always, more soon. Hopefully sooner than it took to get this to you!

Like what you’re reading and want to financially support this journey? One easy way is a one time contribution through Buy Me A Coffee. Every bit helps, but beyond that we are just grateful you’re here with us. Have a Plucky Day!