Tell Me More About Transplants
All about Michael’s Bone Marrow Transplant!
From the day we found out Michael had Mixed Phenotype Acute Leukemia (MPAL) and positive for the Philadelphia Chromosome (Ph+), we knew the best case for long term survival was a bone marrow transplant. Chemotherapy, radiation, and targeted therapies (like the TKI inhibitor drug) can push him into remission for a while, but without a transplant relapse usually happens very quickly, measured in months, not years.
A transplant, even of stem cells, is a serious thing which carries crazy risks. When Michael and I found out about the procedure and what “success” may look like, we cried for quite awhile in the hospital. To even qualify for the transplant, you have to be in general good health to begin with, as the process is brutal on nearly all your organs, from skin to liver. All of Michael’s treatments, like chemotherapy and radiation, have come with tests to make sure he was strong enough to go through them. Of course, the transplant tests were the most grueling and comprehensive, which makes sense as the process is punishing and not possible for the frail of mind or body.
It is a common misconception that a bone marrow, or stem cell transplant, is an operation where the bone marrow is surgically replaced.
The actual procedure is an intravenous infusion of Hematopoietic Stem Cells (the immature stem cells made in our bone marrow which can become any type of blood cell) rather than an injection of actual bone marrow (the soft, spongy material in the center of our bones). The more precise term for what Michael had is Hematopoietic Stem Cell Transplant, or HSCT, but it is most commonly called a Bone Marrow Transplant.
In the past, these stem cells would have been harvested through a process where the donor was put under general anesthesia and then fluid slowly removed using large needles pushed into the top ridge of the rear side of both hip bones. More recent advancements have allowed Hematopoietic Stem Cells to be harvested from the peripheral blood… the blood that is flowing through our bodies.
In the days leading up to the transplant, both donor and recipient go through some treatments. For our son Benjamin, Michael’s haploidentical (half-identical) donor, he needed to have twice daily injections of a medication called filgrastim for three days. These injections stimulate hematopoietic cell production to a point where there’s so much they overflow the bone marrow and freely circulate in the blood, making them much easier to collect.
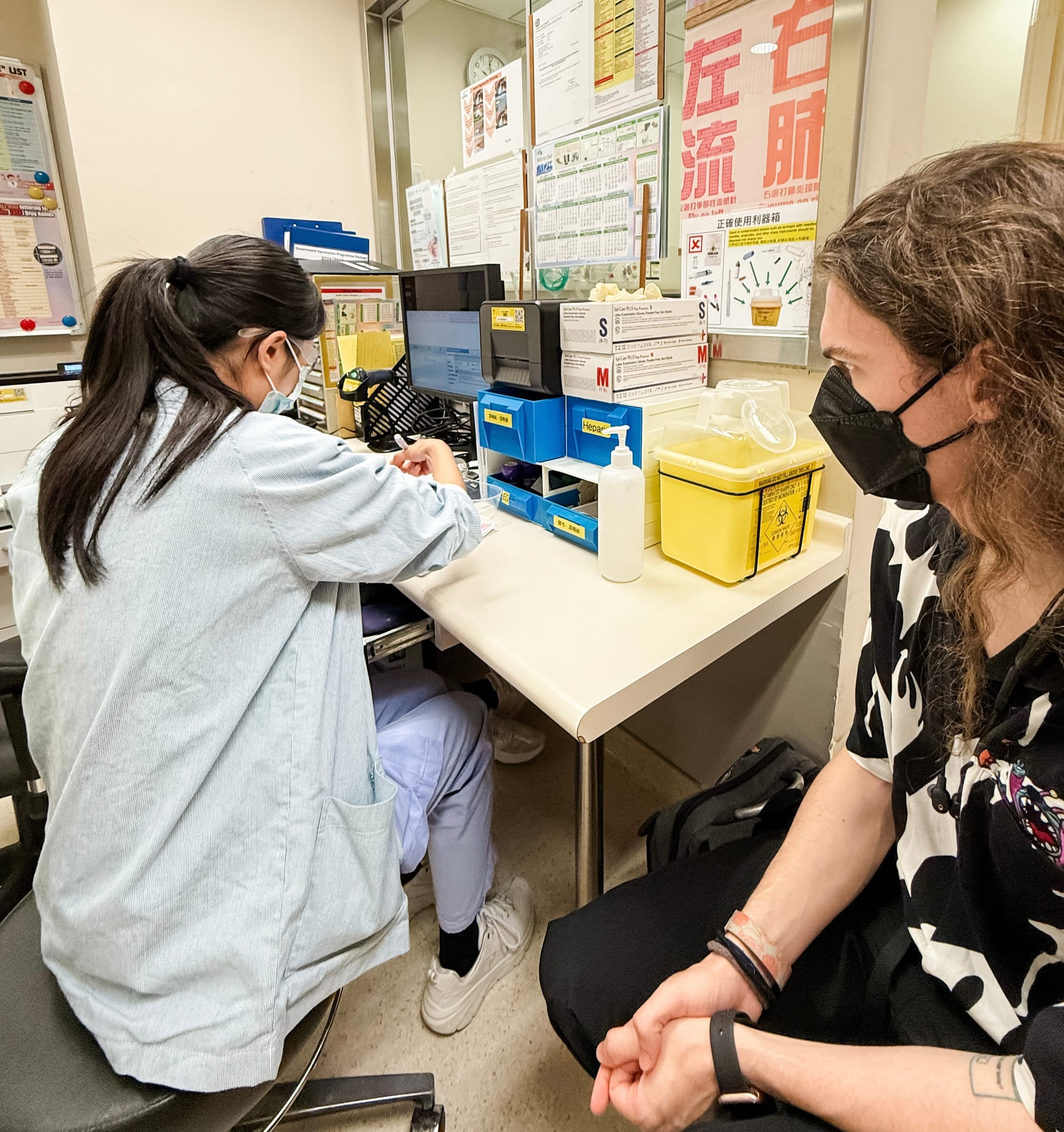
While Michael has previously taken these injections when his white blood count was very low, self-injecting at home, Ben’s were more carefully monitored. He had to go to either a General Outpatient Clinic or the Transplant Ward at Queen Mary Hospital to have the injections done and have them documented on multiple sheets of paper. Because the Hong Kong Government covers 100% of the cost for donors, it makes sense that they want the donation to be as successful as possible and therefore leave no room for error on the donor’s part. His first injection fell on a Sunday morning when almost all of the clinics are closed. We travelled to Yau Ma Tei to a local clinic, arriving right when it opened so the injection could happen during the specified window of time. They were super quick, we were in and out within minutes.
For the Sunday evening injection, all clinics throughout Hong Kong were closed, so we had to go to Michael’s ward. We were able to visit with him before Ben got his second injection. The next day we went to the nearby hospital on our island, and it took eight different people over an hour to figure out what to do, and how to do it! I was so stressed, worried we’d miss the window of when the injection needed to happen. When we went back later for the evening injection they remembered us and we were in and out quite fast. Ben did have some side effects from the injections within one day. He started feeling a low ache in his hips and back, which increased to all of the bones in his body over the next two days. The nurse had told us he might feel “flu-like symptoms,” Ben described it as if his bones were full or bursting.
On Michael’s side, he had three days of chemotherapy followed by three days of full body radiation, including on the day of the transplant. The radiation was done twice a day, in the morning and afternoon. These two therapies combined to kill off any remaining cancer cells along with Michael’s faulty bone marrow to make space for new cells, while also suppressing his immune system so it wouldn’t immediately reject the new donated cells. The isolation ward he’s in and all the precautions we have to take made so much more sense when we realized how he truly won’t be able to fight off any type of infection.
On the morning of Day Zero (transplant day in Leukemia lingo), Ben checked into the Day Ward on Michael’s floor. One IV was placed in one of Ben’s arms and a second one was placed in his opposite hand. During a six hour long procedure, his blood was collected through the IV in his arm, which had to remain straight and still for the entire time. He’d brought his Switch to pass the time playing games, but that was quickly shown to be an impossible task. All the blood was then passed through an apheresis machine which separated the stem cells, collecting them in a sterile bag. The rest of Benjamin’s blood components were returned back to him through the IV in his hand.
For a general overview of what the collection process is like, check out this video. Not everything in the video is applicable to our situation, including the storage part (Ben’s cells were almost immediately transfused into Michael) but it will give you a good idea of the collection part.
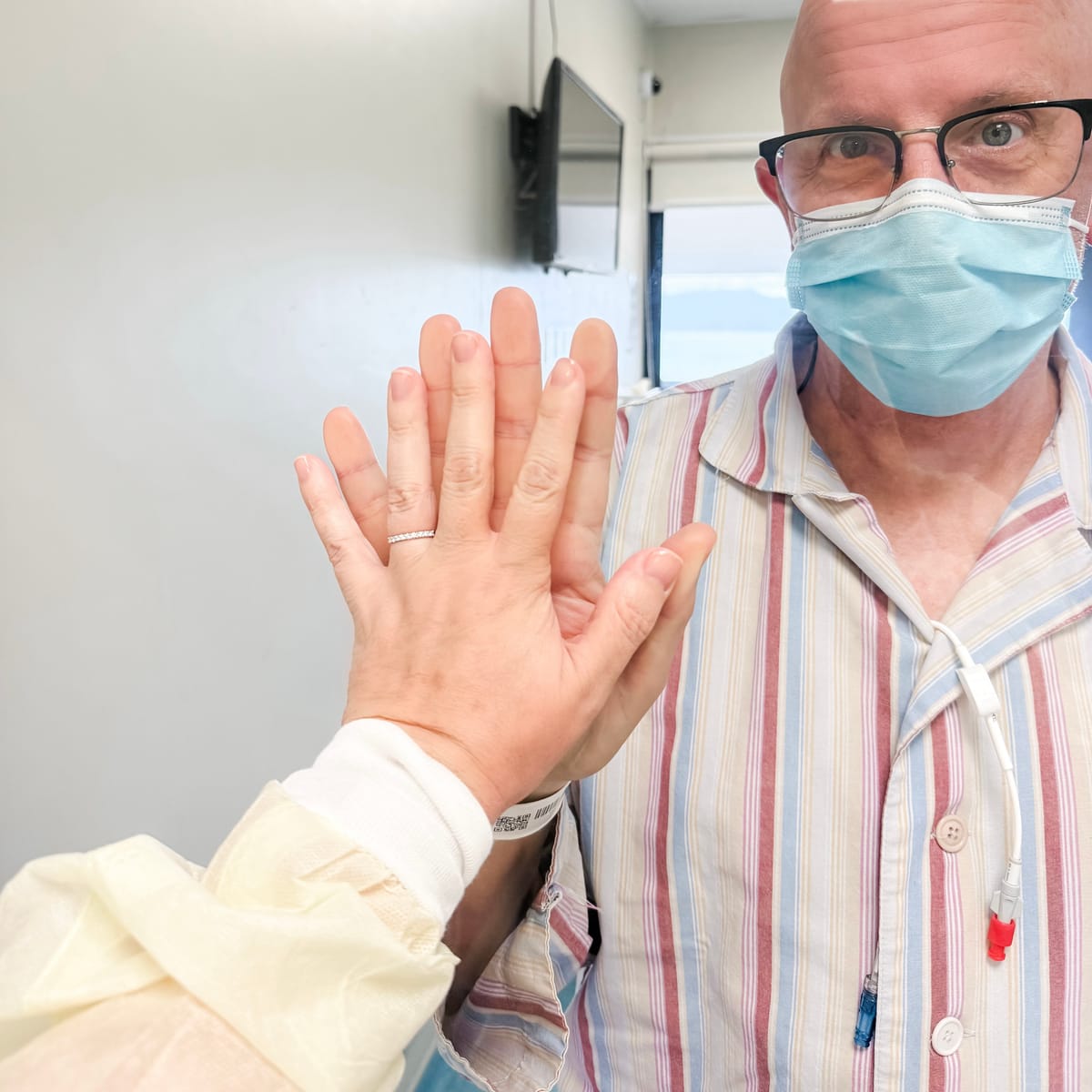
After six hours, Ben said he felt like a raisin, totally depleted of fluids. I brought him a banana and some electrolytes and together we stared in shock at his hand from the arm where the blood was taken… it was swollen to twice the size of his other hand! He also felt very weak all over, so it was a challenge to stand up and get moving after so much time laying flat.

We were told the stem cells would be taken to the lab so they could estimate if they had collected enough in one day, and they’d call at 5:00 pm if he needed to come back the next morning to repeat the process. Because Ben weighs less than Michael, we’d been told it was unlikely they’d get enough the first time around, so they reserved both a second and third day just in case. I booked a room at the nearest hotel, just a three minute ride from the hospital, so we could get Benjamin laying down flat and resting almost immediately following the deeply taxing procedure (shout out to the manager at the Le Méridien Hotel in Cyberport, who ultimately comped part of our stay when I left an honest review on their food and beverage services — it should never be that hard to get a simple cup of coffee! Everything else was okay, especially the close proximity to Queen Mary Hospital.).
Two hours later, the hospital called and said Ben definitely needed to come in again the next day, which meant a return that night for another injection of the filgrastim. He was weak, achey, and exhausted, but we took a three minute taxi ride back (so much shorter than the ninety minutes from our home!) so he could get the injection and then briefly pop in to give his Dad a hug when the evening visiting hour began. Our oldest son also arrived, allowing our whole family to be nearby during this life changing, hopefully life saving, moment.
While the blood in a blood transfusion is bright red, and plasma for a platelet transfusion is an opaque yellow like chicken soup, the Hematopoietic Stem Cells were dark red, almost like BBQ sauce. I don’t know what I thought it would look like… maybe a glittery gold like the precious treasure it is!
While it took six arduous hours on Ben’s side to collect approximately two-thirds of the total volume needed, it took only thirty minutes for the actual transfusion of the stem cells into Michael’s Hickman Line. Benjamin had already gone back to the hotel to lay down and rest, our oldest son sat in the chair next to Michael, casually discussing Star Wars, and I stood in the vestibule trying to make sense of my feelings.
We were at the point of no return.
The literal “valley of the shadow of death.” Michael’s own bone marrow had been destroyed through the radiation, his immune system wiped out through the chemotherapy. These new cells were necessary for Michael to survive. Heavy, scary thoughts. And yet, it all felt a bit anticlimactic to me. Maybe I was waiting for the appearance of a marching band playing a bombastic tune, a proclamation from the mayor with a key to the city, a one hundred member choir singing the Hallelujah Chorus… something more than just a simple bag of fluid casually dripping into Michael’s chest. They did get every single drop, forcing saline into the stem cell bag to flush all that hard-won harvest into his system until the bag was completely emptied.

Through the night they checked on Michael in 15 to 30 minute increments, checking his blood pressure and making sure he wasn’t having any immediate adverse effects. I mentioned in the previous post that I slept deeply that night, I didn’t mention that I kept my phone in my hand so that if anything went wrong, I could get there in minutes. Instead, Michael was bright and perky the next morning while I took a depleted Benjamin back to the Day Ward for a second day of donating.
This time it was much faster, but also a bit more rough, as Ben already felt quite empty. This time they swapped arms and he came a little more prepared with an audiobook preloaded on his phone so he could just lay still with his eyes closed. He was done in four hours, and the staff said the final call would be up to the lab, but it looked like two days of donations would be enough. Benjamin taxied all the way home to minimize the amount of standing or walking he would have to do to be able to climb into his bed, where he would spend the next two days recuperating.
I just want to pause here and express our deep gratitude to everyone who has financially supported us recently. Taxis are expensive and a hotel room is not a typical expense in our budget. But these two items were extraordinarily helpful in making a difficult experience quite a bit more manageable in a tangible way. Thank you!
I waited at the hospital to be with Michael for the evening visiting hours, but they’d already given him the second day’s transplant of Ben’s donated cells before the visiting time arrived. Once again, it all felt incredibly anticlimactic.
After the new, healthy stem cells were transfused into Michael, he was given a couple days just to rest. The effects of the three days of chemo and six sessions of full body radiation were starting to take their toll, and he was told to just lay low in bed and try to sleep. Of course doctors and nurses were constantly checking on him, making it a little difficult, but he did his best to snooze when he could.
Then it was time for the next step of the process, two days of the most potent chemotherapy Michael has received yet. This was the part which would truly wipe out and fully suppress the last of Michael’s immune system, giving all those fresh cells plenty of space to take root and start growing while Michael’s blood counts (red blood cells, white blood cells, neutrophils, and platelets) all hit as close to zero as they can get in the hopes of kickstarting the new stem cells into production.
Today Michael is on Day Ten following the transplant. Yesterday and today his platelets were down to ten (normal is 150 to 400, emergency danger zone is under 50) so he got a plasma/platelet transfusion (the chicken soup-like substance) to keep him from serious complications.
We were told that by Day Twenty we’ll know if the transplant is a success or not, and then we’ll enter the next phase of the process, the delicate balancing act of suppressing Michael’s immune system just enough to not reject the transplant while letting it get used to working just a little bit before he can safely leave isolation. Right now, Ben’s cells are flowing through Michael’s bloodstream, migrating toward his destroyed bone marrow and hopefully beginning to get busy in rebuilding healthy new bone marrow.
Next up we’ll work on explaining some of the expected transplant side effects Michael is already experiencing. The last couple of days were emotionally difficult for Michael, but the next few days are going to be extremely physically rough. Every doctor and nurse who enters his room reminds him of how hard it’s going to get before it will (please God) get better. It’s remarkable how close to death they need to bring you before new life can begin. Even Benjamin felt like he had been nearly drained of his life to be able to give his Dad a chance at a longer one.
June 30th was Ben’s 22nd birthday. We’d already celebrated a couple weeks prior, knowing Michael would be in the hospital, post-transplant. Benjamin’s birthday wish was for his Dad to survive, and through his rough donation process he is doing so much to actively make that wish come true. What a GIFT Ben is to all of us!

Want to support more of this content? Be sure to subscribe so you can get these newsletters delivered directly to your email inbox! For a one time support option, consider a contribution through Buy Me A Coffee. Every bit given here goes to meeting practical needs, like transportation or sustenance. No pressure! We’re just glad you’ve joined us on this Plucky Day!